Make it Free? –
DEC. 16, 2020 – “SADLY, THE DRUG OVERDOSE EPIDEMIC CONTINUES, AND IT HAS BECOME MORE COMPLICATED DURING THE COVID-19 PANDEMIC,” SAID PATRICE A. HARRIS, M.D., M.A., CHAIR OF THE AMA OPIOID TASK FORCE. “IT IS LONG PAST DUE FOR ALL STAKEHOLDERS TO REMOVE BARRIERS TO CARE AND ADDRESS SYSTEMIC INEQUITIES THAT HAVE BEEN BROUGHT TO LIGHT DURING THIS PANDEMIC. PHYSICIANS AND OTHER HEALTH CARE PROFESSIONALS WILL CONTINUE TO TAKE ACTION, AND THE AMA IS WILLING TO WORK WITH ALL STAKEHOLDERS TO IMPLEMENT THESE RECOMMENDATIONS TO PREVENT FUTURE DEATHS.”
“The recommendations laid out in this year’s analysis build on our work from 2019 and elevate proven solutions,” said Joel Ario, managing director, Manatt Health, and former insurance commissioner in Oregon and Pennsylvania. “Still, we have an unprecedented public health challenge today, as the COVID-19 pandemic has strained our health care system, exacerbated the drug overdose epidemic, and highlighted pre-existing, systemic barriers to care facing vulnerable and underrepresented populations.”
The AMA and Manatt recommendations come amid five key themes surrounding the current drug overdose epidemic:
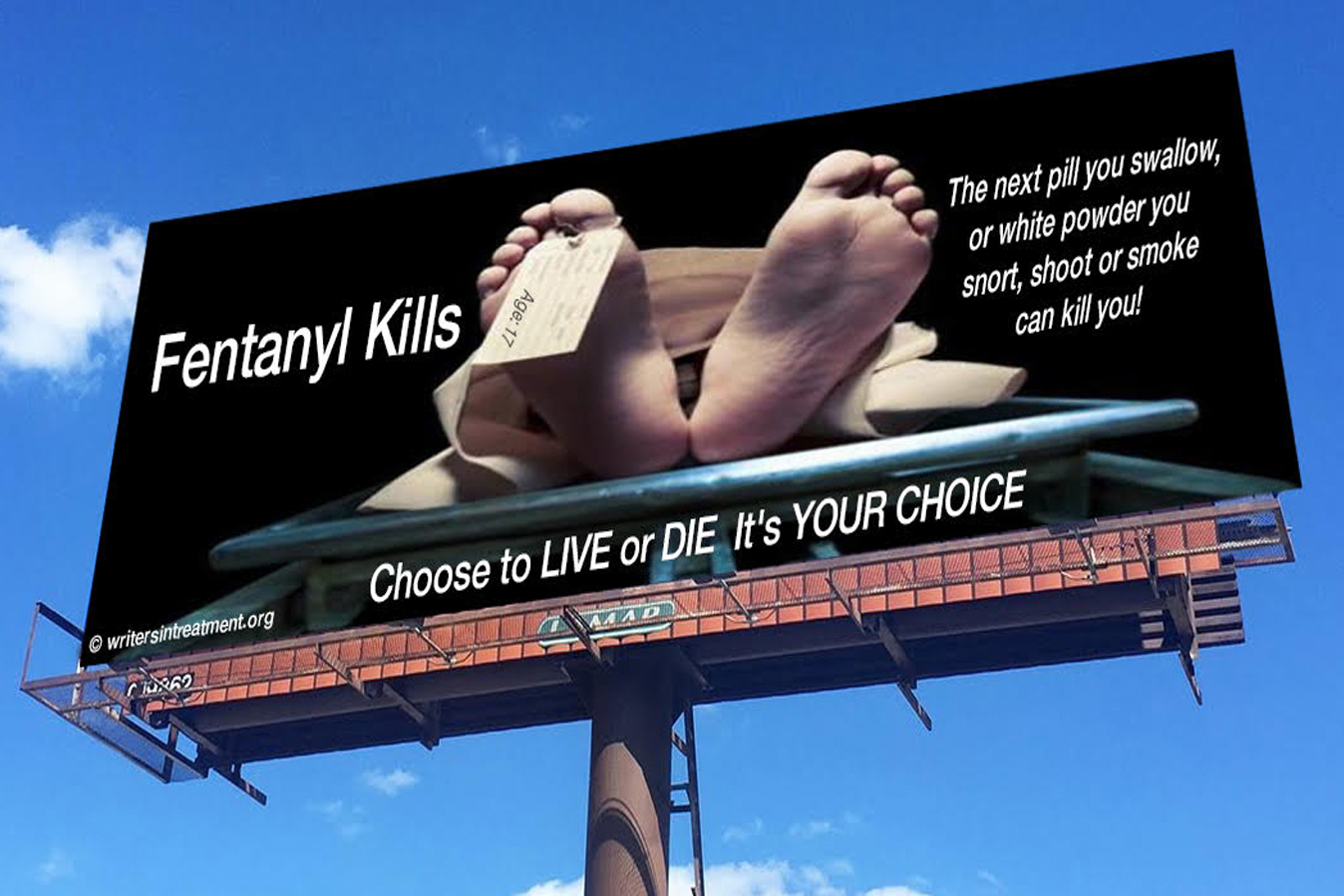
An evolving drug overdose epidemic. The “opioid epidemic” continues to evolve into a more deadly and broader drug overdose epidemic, with more people dying from illicit fentanyl, heroin, cocaine, and methamphetamine even as opioid prescribing has decreased by nearly 40 percent in the past six years. According to the CDC, from the beginning of 2015 to the end of 2019, the number of deaths involving illicitly manufactured fentanyl and fentanyl analogs increased from 5,766 to 36,509, while deaths involving prescription opioids decreased from 12,269 to 11,904. Simultaneously, increased stress, social isolation, and disruptions to treatment plans during the pandemic has made access to treatment more complicated.
Communities of color face higher risks. Despite experiencing rates of SUD similar to those of white Americans, Black Americans and other minoritized and marginalized populations experience sharp disparities in access to SUD treatment due to a range of factors, including stigmas that Black Americans are more likely to use illicit substances and feel less pain, a mistrust of the health care system by Black Americans, and a shortage of health care professionals and opioid treatment programs in those communities.
Mental health and substance use disorder treatment are linked. The COVID-19 pandemic has demonstrated the link between mental health and substance use disorder. While some states have enacted meaningful laws—and 30 states have joined a new National Association of Insurance Commissioners working group to refine regulatory tools that can hold insurers accountable—state and federal oversight remains limited. When states conduct compliance exams, they routinely find parity violations.
Telehealth. One implication of the COVID-19 pandemic has been the rapid expansion of telehealth services. Ensuring behavioral health and SUD providers receive full reimbursement for these virtual services has become an essential aspect of continued treatment plans during the pandemic, and it will likely remain important in the future. While telehealth access should not be viewed as a substitute for an adequate in-person provider network, the changes made by the U.S. Drug Enforcement Administration and SAMHSA to help individuals maintain access to critical services during the COVID-19 pandemic should be continued.
Justice-involved populations are overlooked. Those who are incarcerated or in drug diversion programs, including those who are incarcerated in part due to substance use disorder or a related mental health issue, face distinct barriers to coverage. As recent lawsuits have validated, corrections officials must provide physician-prescribed medications for opioid use disorders to incarcerated individuals. In addition, once these individuals are released, it is vital they have access to harm reduction strategies and continued treatment plans.